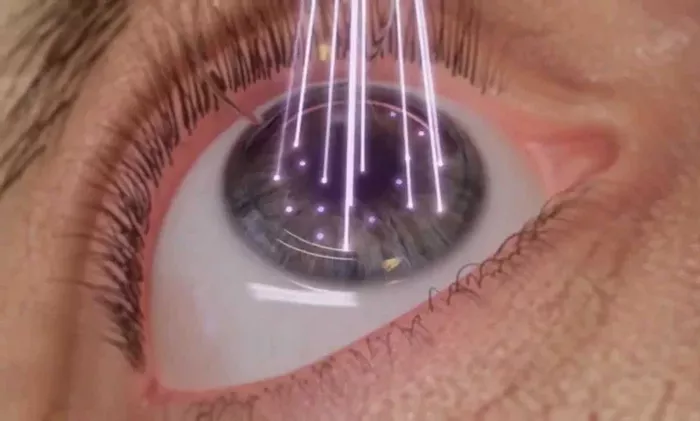
Eye transplant surgery, also known as corneal transplant surgery or keratoplasty, is a highly specialized procedure aimed at restoring vision in patients with damaged or diseased corneas. The cornea is the clear, dome-shaped surface that covers the front of the eye and plays a crucial role in focusing light onto the retina. When the cornea becomes cloudy or scarred, it can significantly impair vision. Eye transplant surgery involves replacing the damaged cornea with a healthy donor cornea. This article outlines the 7 major steps in eye transplant surgery, providing an in-depth look at the procedure and what patients can expect.
Step 1: Preoperative Evaluation and Preparation
Patient Assessment
The first step in eye transplant surgery is a thorough preoperative evaluation. This assessment includes a detailed medical history, eye examination, and various tests to determine the extent of corneal damage and the suitability of the patient for surgery.
Medical History
The ophthalmologist will review the patient’s medical history to identify any underlying health conditions that could affect the surgery or recovery. Conditions such as diabetes, autoimmune diseases, and infections must be carefully managed.
Eye Examination
A comprehensive eye examination is performed to assess the health of the entire eye. This includes measuring visual acuity, examining the cornea with a slit-lamp microscope, and checking intraocular pressure. The ophthalmologist will also evaluate the retina and optic nerve to ensure they are healthy.
Specialized Tests
Several specialized tests may be conducted, including:
Corneal Topography: Maps the surface curvature of the cornea to identify irregularities.
Pachymetry: Measures corneal thickness.
Specular Microscopy: Evaluates the health of the corneal endothelium, the innermost layer of the cornea.
Donor Tissue Matching
Matching the donor cornea to the recipient is crucial. The donor cornea is obtained from an eye bank, where it is carefully screened for infections and other issues. Tissue typing and blood compatibility tests are performed to reduce the risk of rejection.
See Also: 5 Types of Eye Surgery Robots
Step 2: Surgical Planning
Choosing the Type of Keratoplasty
There are different types of corneal transplants, and the choice depends on the extent and location of corneal damage. The main types are:
Penetrating Keratoplasty (PK): Full-thickness transplant where the entire cornea is replaced.
Lamellar Keratoplasty (LK): Partial-thickness transplant where only the damaged layers of the cornea are replaced. It includes:
Deep Anterior Lamellar Keratoplasty (DALK): Replaces the front and middle layers of the cornea.
Descemet’s Stripping Endothelial Keratoplasty (DSEK): Replaces the inner layers, including the endothelium.
Descemet Membrane Endothelial Keratoplasty (DMEK): Replaces only the innermost layer.
Surgical Approach
The ophthalmologist will plan the surgical approach, including the incision size and location, and determine the type of anesthesia to be used. Local anesthesia with sedation is commonly used, but general anesthesia may be necessary for some patients.
Patient Preparation
Patients are advised to stop taking certain medications, such as blood thinners, prior to surgery. They are also instructed to fast for several hours before the procedure. The eye is cleaned and sterilized, and the patient is prepped for surgery.
Step 3: Donor Cornea Preparation
Obtaining Donor Tissue
The donor cornea is obtained from an eye bank. It is screened for infectious diseases and other issues. The cornea must be harvested within a few hours of the donor’s death to ensure viability.
Cornea Storage
The donor cornea is stored in a special solution that preserves its viability. It is kept in a sterile environment to prevent contamination.
Preparation for Transplant
Just before the surgery, the donor cornea is carefully inspected and prepared. The donor cornea is cut to the appropriate size and shape using a trephine, a surgical instrument that creates a circular incision.
Step 4: Removal of the Damaged Cornea
Creating the Incision
The ophthalmologist makes a precise incision in the patient’s cornea using a trephine. The size and shape of the incision depend on the type of keratoplasty being performed. For penetrating keratoplasty, a full-thickness incision is made. For lamellar keratoplasty, a partial-thickness incision is created.
Removing the Damaged Tissue
The damaged corneal tissue is carefully removed. In penetrating keratoplasty, the entire cornea is removed. In lamellar keratoplasty, only the affected layers are excised, leaving the healthy layers intact.
Preparing the Surgical Site
The surgical site is prepared for the placement of the donor cornea. The ophthalmologist ensures that the edges of the incision are clean and smooth to facilitate proper healing.
Step 5: Implantation of the Donor Cornea
Positioning the Donor Cornea
The prepared donor cornea is placed onto the patient’s eye. The ophthalmologist ensures that the donor tissue is correctly positioned and aligned with the patient’s natural cornea.
Securing the Donor Cornea
The donor cornea is secured in place using fine sutures. The type of sutures and the suturing technique depend on the type of keratoplasty. For penetrating keratoplasty, interrupted or continuous sutures may be used. For lamellar keratoplasty, fewer sutures may be needed.
Adjusting Sutures
The ophthalmologist adjusts the sutures to ensure the donor cornea fits snugly and evenly. Proper tension is crucial to prevent astigmatism and promote healing.
Step 6: Postoperative Care and Monitoring
Immediate Postoperative Care
After the surgery, the patient is taken to a recovery area. The eye is covered with a protective shield to prevent injury and infection. The patient is monitored for any immediate complications.
Medications
Patients are prescribed medications to prevent infection and reduce inflammation. These may include:
Antibiotic Eye Drops: To prevent infection.
Steroid Eye Drops: To reduce inflammation and prevent rejection.
Pain Relievers: To manage discomfort.
Follow-Up Appointments
Regular follow-up appointments are scheduled to monitor the healing process and detect any complications early. The ophthalmologist will check for signs of rejection, infection, and other issues.
Suture Management
Sutures may need to be adjusted or removed over time. The timing of suture removal depends on the type of keratoplasty and the individual healing process.
Step 7: Long-Term Recovery and Outcomes
Healing Process
The healing process varies for each patient. It can take several months to a year for the eye to fully heal and for vision to stabilize. Patients need to be patient and follow their ophthalmologist’s instructions closely.
Vision Improvement
Most patients experience significant improvement in vision after corneal transplant surgery. However, some may need glasses or contact lenses to achieve the best possible vision. In some cases, additional procedures such as laser surgery may be necessary to correct refractive errors.
Complications and Risks
While corneal transplant surgery is generally safe, there are potential risks and complications, including:
Rejection: The immune system may recognize the donor cornea as foreign and attack it. Prompt treatment with medications can often manage rejection.
Infection: Proper postoperative care and medication can minimize this risk.
Astigmatism: Irregular curvature of the cornea can result from the surgery, sometimes requiring additional correction.
Lifelong Care
Patients who undergo corneal transplant surgery require lifelong care and monitoring. Regular eye exams are essential to ensure the continued health of the transplanted cornea and to detect any issues early.
Quality of Life
Successful corneal transplant surgery can significantly enhance a patient’s quality of life by restoring vision and improving daily functioning. It is important for patients to maintain a healthy lifestyle and follow their ophthalmologist’s recommendations to preserve their vision.
Conclusion
Eye transplant surgery is a complex but highly effective procedure for restoring vision in patients with damaged or diseased corneas. Understanding the seven major steps involved—from preoperative evaluation to long-term recovery—can help patients prepare for the journey ahead. With proper care and monitoring, many patients achieve significant improvements in vision and quality of life.
Related topics: